Screening & Testing

SCREENING & TESTING
Part of being proactive about your health, whether you are cancer-free, currently in treatment, or a survivor, is scheduling regular screening and testing appointments with your doctor. Also, it’s very important to ensure that you understand what specific tests are for and why your doctor may order these tests. Tests fall into three categories:
- Screening tests:These tests, such as a yearly mammogram, are given to determine if there is any evidence of breast cancer in a seemingly healthy person. Being proactive and having screening tests enables you and your doctor to notice any differences in your breasts, and if there are any issues, then you can address any symptoms as early as possible.
- Diagnostic tests:If it has been determined that you may have cancer, a diagnostic test can determine if you have cancer or not. In addition, if it is evident that you do have cancer, diagnostic tests can determine if your cancer has spread beyond your breast. These tests can give your doctor more information about your cancer, which can help your doctor design the best course of treatment for you.
- Monitoring tests: After you have been diagnosed with cancer, monitoring tests determine how well the treatments are working. Also, these tests can determine whether your cancer has returned or not.
The following list consists of all three categories of tests, listed in alphabetical order:
Biopsy: Although physical exams and MRIs can determine if there is a lump or mass in your breast, a biopsy is an actual sampling of the tissue of the lump or mass. By sampling the tissue, the tissue can then be examined by a pathologist, who can determine if the mass is cancerous, and can create a pathology report with all of the details. A biopsy is usually minimally invasive and involves numbing the breast with local anesthesia and then inserting a tiny needle to obtain samples of tissue from the lump. Sometimes biopsies involve making a small incision to obtain a sample.
Blood Cell Counts: Your doctor may order a blood cell count test to be done at any time, before your treatment, or during your treatments. These tests check the numbers of cells you have. White blood cells guard against infection, and if they are low, you are more susceptible to infection. Red blood cells bring oxygen to various parts of the body; if the level of hemoglobin is low, that can be indicative of anemia. Platelets help your blood clot. Before you can start any treatment, your doctor has to make sure that you are not anemic, so this blood cell count test will be given to you. Also, at the beginning of every chemotherapy session you may have, your doctor will have you take another blood cell count test to ensure that your blood cell counts are normal.
Blood Chemistries: In order to determine if your organs are functioning well during your treatment, your doctor may order a blood chemistries test. This test measures things like potassium levels, blood sugar and calcium levels, among others, to determine if your body is functioning well.
Blood Marker Tests: Your doctor may order these tests at any time: before, during, or after treatment. These tests measure proteins that a cancerous tumor emits, and also test for cells from the tumor that may be circulating throughout the body. The disadvantage of these tests is that they are not always conclusive, sometimes requiring additional tests, and they can be expensive.
Bone Scans: You may have to have a bone scan either before you initially begin any treatment, to see if your bones are healthy, or possibly during your treatment, if there is a concern that the cancer has spread to your bones. A bone scan involves a radioactive injection in your arm, which is absorbed into the bones, and then your body is scanned to see the activity in your bones. This test is painless, aside from the initial injection.
Breast Cancer Index Test: Although not currently approved for use by the U.S. Food and Drug Administration, this test determines the likelihood of node-negative, hormone-receptor-positive breast cancer recurring within five to ten years after the initial diagnosis. This is done by analyzing seven specific genes. Your doctor can use this test to determine if hormonal therapy will be beneficial for an additional five years. http://www.breastcancer.org/symptoms/testing/types/breast-cancer-index-test
Breast MRI (Magnetic Resonance Imaging): An MRI enables your doctor to get a cross-sectional view of your breast, which is done through an MRI machine that uses magnets and radio waves to create this picture.
Breast Physical Exam: This is a physical exam that should be done by your doctor on a yearly basis in order to detect any abnormal lumps. For those in treatment, your doctor will recommend a physical exam about every three to four months.
Breast Self-Exam (BSE): This exam involves examining your own breasts once a month to determine if there are any irregularities in your breast. After examining your breasts for a regular period of time, you will learn what is “normal” for you and what, possibly, is not normal. This should be done in conjunction with regular doctor visits and physical exams.
CT (CAT) Scans (Computerized Tomography): These tests may be ordered for you to determine if your breast cancer has spread beyond the chest wall or to other parts of your body. This scan provides a two-dimensional picture of your body, which is done by having a dye injection first, then lying on your back while being moved through a circular-shaped machine.
Chest X-Rays: Your doctor may order a chest x-ray (in the case that you have invasive breast cancer) to see if the cancer has spread to your lungs. Other uses may be to determine if you have pneumonia or other possible lung issues during treatment.
Digital Tomosynthesis: This is a newer test which provides a three-dimensional picture of the breast using x-rays. It is done similarly to a mammogram, but with a lot less pressure than a mammogram. The advantage of this test is that is provides a three-dimensional picture, while a mammogram only provides a two-dimensional picture of the breast.
Ductal Lavage: This test involves using inserting a small tube into the milk duct, and then fluid is washed into the duct, rinsing out the duct and its cells. The fluid is drawn out through suction to the nipple. The fluid and the cells are then examined at a lab. If cancerous cells are found, your doctor will order additional tests.
EndoPredict Test: This test analyzes a set of genes, which can indicate how your cancer will act and how treatment will affect your cancer. This can affect how your doctor determines your course of treatment. Unfortunately, this treatment is not available in the U.S., and is only available in Europe currently.
FISH Test (Fluorescence in Situ Hybridization): This test maps the genetic material in tissue extracted during a biopsy. This is done to determine if the cells have excess copies of the HER2 gene. Excess copies of this gene indicate that there are more HER2 receptors in the cells; these HER2 receptors function to accept signals that increase breast cancer cell growth. Essentially, this test shows if the cancer is positive or negative for HER2.
IHC Tests (ImmunoHistoChemistry): This test, which is done by staining cancer tissue obtained from a biopsy, determines if there are HER2 receptors and/or hormone receptors on the cancer cells. Your doctor will use this information in planning your cancer treatments.
Inform HER2 Dual ISH Test: This test, which is short for “in situ hybridization” involves the staining of tissue, which causes the HER2 proteins in a tissue sample to change color, which is visible under a microscope. This test will determine if the breast cancer cells are HER2 positive. HER2 positive breast cancer is a type of cancer where the HER2 proteins are too high, which encourages breast cancer to grow.
MammaPrint Test: This test is performed on breast cancer tissue that was removed in a biopsy. Intended for early-stage breast cancer patients, the test analyzes the activity of specific genes. Eventually, this test may be used to determine the risk of recurrence in the patient within 10 years of the initial diagnosis.
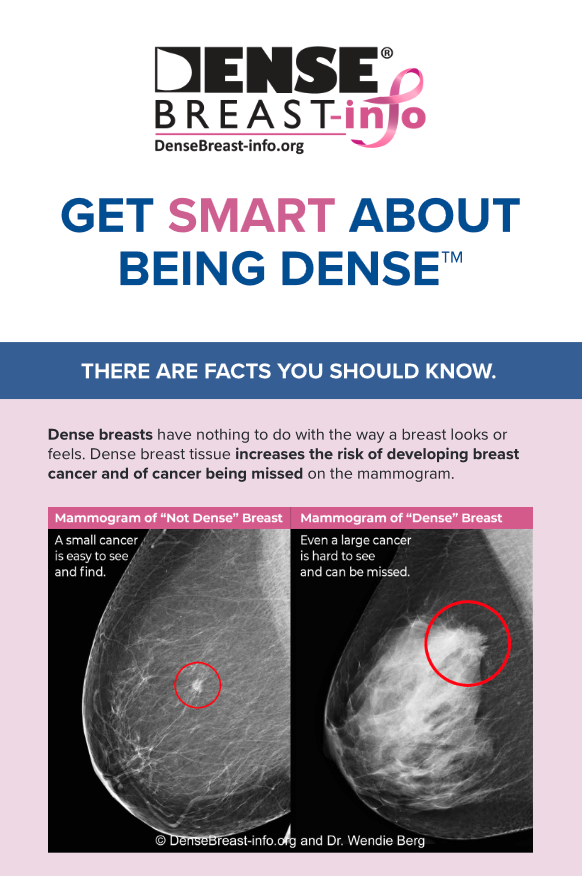
Mammograms: In use for over 50 years, this is a safe and easy way to take a two-dimensional x-ray of the breast. Women 40 years of age and over should have an annual mammogram.
Mammostrat Test: This test measures the presence of five specific genes in early-stage hormone receptor-positive breast cancer cells. The results of this test can help determine if the cancer will come back, and doctors can tailor your treatments based on the likelihood that the cancer will return.
MarginProbe: When a surgeon removes a lump during a lumpectomy, the tumor is removed, as well as some tissue around the lump. A MarginProbe can identify other cancerous tissue within three to five minutes by using electromagnetic waves during the lumpectomy, so the surgeon can remove this tissue during the lumpectomy, which can reduce the risk of having to have a second surgery to remove more tissue.
Molecular Breast Imaging: This test begins with the injection of a radioactive substance via the arm. Breast cancer cells will absorb this substance faster than regular cells, so it makes it easier to see these cells when the body is scanned by a nuclear medical scanner.
Oncotype DX Test: This test uses gene analysis to determine how two different types of cancer will respond to treatment. The first way this is used is to see how likely it is that early-stage estrogen-receptor-positive breast cancer will return, and also to see if post-surgical chemotherapy will be effective for this type of cancer. The second way this test is used to see how likely it is that ductal carcinoma in situ (DCIS) will return, and/or if there is the likelihood of a new invasive cancer will start in the same breast. Also, this includes the probability of the effectiveness of post-surgical radiation therapy.
PET Scans: This type of test is not used for screening for cancer, but instead is used to see if: the cancer has moved to the lymph nodes; is metastatic; or to see if the treatment is having an effect on metastatic cancer. PET stands for Positron Emission Tomography, which starts with an injection of a combination of sugar and radioactive material. Cancer cells will take in more of the radioactive sugar material, since these cells are more active than regular cells. As a result, the cancerous cells will be more visible when they are scanned during this test, which will then show areas of possible cancer.
Prosignia Breast Cancer Prognostic Gene Signature Assay: This gene test looks at early-stage hormone-receptor-positive breast cancer genes and their activity. Essentially, this test can determine a woman’s risk of recurrence over five years after the initial diagnosis, which can help a doctor decide if five or ten years of hormone therapy is appropriate for her situation.
SPoT-Light HER2 CISH Test: This test, called Subtraction Probe Technology Chromogenic In Situ Hybridization determines if breast cancer cells are HER2-positive. Testing as HER2 positive means that there is an abundance of HER2 receptor proteins on the surface of the cells; these receptors help the cell grow and multiply.
Thermography: This test uses thermal imaging to find tumors. This is based on the thought that a tumor contains rapidly reproducing cells, which increases the blood flow to a cell, which can raise the temperature of the skin. This test can be used to supplement a mammogram but should not be used in place of a mammogram.
Ultrasound: An ultrasound uses sound waves to create an image. This test may be ordered if a lump has been detected through a mammogram or through a physical exam. An ultrasound is helpful in determining if a lump is a solid lump, or if a lump is actually a cyst or a fluid-filled sac.
Urokinase Plasminogen Activator Protein Inhibitor Test: This test is performed on tissue that is taken during a biopsy. This Urokinase Plasminogen Activator Protein Inhibitor helps cancer spread and multiply, and can be found on the exterior of a breast cancer cell. Often this test is performed in women who have hormone-receptor-positive, HER2-negative breast cancers that haven’t spread to the lymph nodes.